Cutting-Edge Health Equity Innovations You Should Know About

Why health equity matters (and how we’re fixing it) in 2025
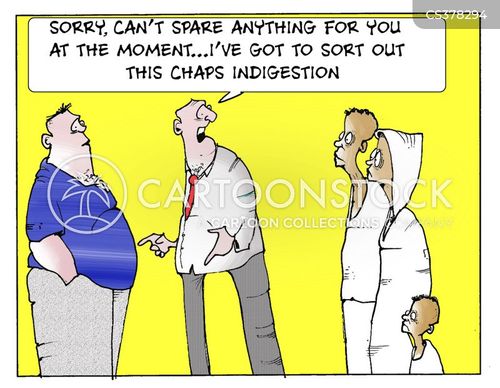
Picture this: You walk into two hospitals with the exact same problem.
In Hospital A, you wait 30 minutes, see a doctor who listens carefully, and leave with effective treatment.
In Hospital B, you wait 3 hours, see a rushed doctor who barely makes eye contact, and leave with generic advice that doesn’t help.
The difference? Maybe your zip code. Or your skin color. Or how much money you make.
That’s the healthcare gap we’re talking about. And in 2025, we’re finally getting serious about closing it.
Health equity innovation is about creating scalable, investable solutions to reduce these disparities. It’s not just about feeling good – it’s actually saving us money. Healthcare inequities cost us $320 billion annually and could exceed $1 trillion by 2040 if we don’t fix them.
So let’s dive into how we’re solving this problem (with my opinion sprinkled on top, of course).
The big health equity trends of 2025

1. AI and data analytics (that actually work)
Remember when “big data” was just a buzzword? Now it’s actually delivering results.
AI tools are helping identify at-risk populations by analyzing not just medical records but also social factors like housing, education, and income. This matters because only about 20% of health outcomes come from clinical care – the other 80% come from these social determinants.
The catch? AI is only as good as the data feeding it. If your dataset is biased (spoiler alert: most are), your AI will perpetuate those biases.
Medical Affairs teams are playing referee here, making sure the fancy AI tools actually help real patients in underserved communities instead of just looking good in investor presentations.
2. Telehealth 2.0
Telehealth isn’t just for pandemic emergencies anymore – it’s become a powerful equalizer for communities that have traditionally been left behind.
In 2025, we’re seeing telehealth evolve beyond basic video calls to include:
- Chronic disease management
- Remote monitoring through wearables
- Mental health support
- Specialized care access for rural patients
One study from the University of Michigan found that telehealth significantly reduced appointment no-shows in underserved communities by eliminating transportation barriers. When patients don’t have to choose between a doctor’s appointment and a day’s wages, everybody wins.
3. Community-driven solutions
The days of top-down healthcare are fading fast. The most successful innovations now come from partnerships with the communities they’re trying to serve.
Take the Health Equity Innovation Challenge, which brings together local leaders, healthcare providers, and tech innovators to create solutions that actually work in real neighborhoods with real people.
These aren’t just feel-good projects – they’re becoming commercially viable models that deliver better health outcomes at lower costs.
4. Smart policy (finally)
In 2025, policy is catching up with reality. Programs like the Health Equity Index (HEI) are giving providers financial incentives to address social determinants and deliver more equitable outcomes.
Medicare Advantage expansions are including coverage for things like healthy food delivery, transportation to appointments, and even housing support – recognizing that these “non-medical” factors actually determine health outcomes.
The most forward-thinking healthcare organizations aren’t waiting for mandates – they’re developing comprehensive outreach strategies that connect with patients where they are, physically and culturally.
Where innovation is making the biggest impact

Chronic disease management
Diabetes, heart disease, and hypertension hit underserved communities harder. Now AI-powered outreach is helping identify high-risk patients before they need emergency care.
Smart wearables are enabling continuous monitoring, with research from Stanford Medicine showing that these devices can detect physiological changes that predict disease flare-ups days before symptoms appear.
Mental health access
Mental health has been healthcare’s neglected stepchild for too long, especially in marginalized communities. Digital therapy platforms are now reaching people who would never set foot in a traditional therapist’s office.
Virtual support groups, culturally tailored interventions, and smartphone-based cognitive behavioral therapy are bridging massive gaps in care. Mental health disparities alone cost $116 billion annually through reduced productivity and increased healthcare costs.
Maternal health equity
Black women are still 3x more likely to die from pregnancy-related causes than white women. That’s not just a statistic – it’s a tragedy.
Digital health platforms focused on maternal care are now connecting expectant mothers with doulas, monitoring high-risk pregnancies remotely, and providing culturally competent education throughout pregnancy and beyond.
The Black Maternal Health Momnibus Act is finally getting the funding and implementation it deserves, addressing systemic issues in maternal care.
How I’m thinking about health equity

After researching this topic, I’ve come to believe that health equity isn’t just a moral imperative – it’s a business imperative too.
Healthcare organizations that ignore disparities are leaving money on the table. They’re paying for preventable emergency room visits, managing chronic conditions that could have been prevented, and missing out on patient populations who could be loyal customers if properly served.
The most successful innovations are:
- Data-driven but human-centered – using AI and analytics while remembering real people are involved
- Community-partnered – not just designed FOR communities but WITH them
- Multisector – breaking down silos between healthcare, tech, community organizations, and policy
- Commercially viable – sustainable models that deliver both social impact and financial returns
What’s next?

The road to health equity is long, but for the first time, it feels like we’re actually making progress.
As innovation continues to accelerate, I expect we’ll see:
- More personalized medicine that accounts for genetic diversity across populations
- Further integration of healthcare with social services
- AI that helps detect and correct for bias in medical decision-making
- Virtual care networks that transcend geographic and economic barriers
The most exciting innovations aren’t just technological – they’re about reimagining the entire healthcare experience from the ground up, with equity built into the foundation rather than tacked on as an afterthought.
As Dr. Martin Luther King Jr. said, “Of all the forms of inequality, injustice in health is the most shocking and the most inhuman.” In 2025, we’re finally getting serious about fixing it.
And unlike most healthcare problems, this is one where everybody wins – patients, providers, and even the bottom line.
The question isn’t whether we can afford to invest in health equity innovation. The real question is: how can we afford not to?