Bringing Medical Device Concepts to Market: Key Challenges and Solutions
The path from a sketch on a napkin to a life-saving device in a patient’s hands is one of the most arduous, painstaking journeys in modern industry. For innovators, the process is a minefield of regulatory hurdles, funding gaps and engineering paradoxes. But in 2025, a new and critical challenge has moved to the forefront: equity.
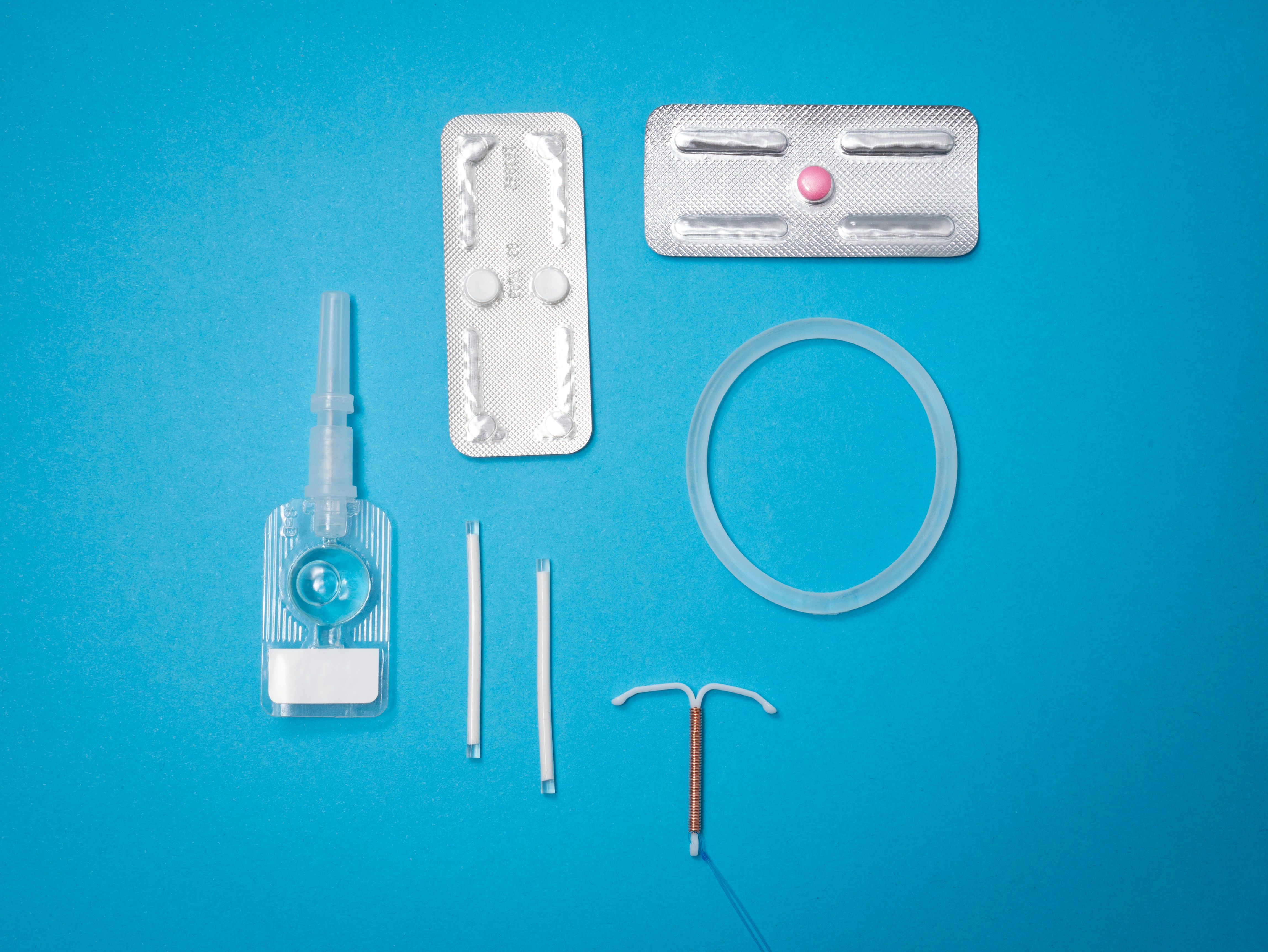
For decades, the metric for a successful medical device was simply safety and efficacy. Did it work? Was it safe? But today the questions are evolving. We must now ask: Who does it work for? As we move toward a healthcare system that prioritizes inclusivity, the process of bringing medical device concepts to market is being rewritten to ensure that innovation benefits every patient, not just a privileged few.
The Challenge of Inclusive R&D
One of the most pervasive issues in the industry has been the “standard patient” fallacy. Historically, devices were designed, tested and validated on homogenous cohorts. typically young, white and male.
The challenge for modern developers is to integrate inclusivity into the very earliest stages of the design lifecycle. This adds complexity. It means sourcing diverse anthropometric data, accounting for varying skin tones in optical sensors and considering how social determinants of health (like internet access for connected devices) affect usability.
The Solution: The industry is moving toward “Co-Design” frameworks. Instead of designing for patients, successful companies are designing with them. This involves establishing community advisory boards early in the concept phase. By engaging with diverse patient populations before a prototype is even built, engineers can identify cultural, physical, or logistical barriers that would otherwise cause the product to fail in the real world.
Navigating the “Valley of Death”
Beyond design, the financial chasm known as the “Valley of Death”, or the gap between initial grant funding and commercial revenue, remains a primary killer of medical innovation. This is particularly true for devices aimed at niche or underserved populations, where the immediate return on investment (ROI) might not attract traditional Venture Capital.
Investors are often risk-averse, and the regulatory pathway for novel devices is long and expensive. A device designed to improve maternal health outcomes in rural areas might struggle to find funding compared to a high-margin elective surgery tool.
The Solution: Strategic partnerships are key. Innovators are increasingly looking toward non-dilutive funding sources, such as government grants focused on health equity (like those from the NIH or NSF) and partnerships with large health systems that are incentivized to reduce long-term care costs. Additionally, as discussed in recent articles on expanding reach of specialized healthcare services with mobile medical vehicles, rethinking the delivery mechanism itself can make a business case more viable. By tying a device to a broader service model (like mobile clinics), developers can demonstrate a clearer path to adoption and reimbursement.
Regulatory hurdles as a Strategic Advantage
For many startups, the FDA submission process is seen as a terrifying final boss. The complexity of the Modernization of Cosmetics Regulation Act (MoCRA), the EU MDR and evolving AI guidance can paralyze a team.
However, the most successful companies treat regulatory strategy not as a hurdle, but as a roadmap. A common mistake is delaying regulatory conversations until the device is fully developed. This often leads to the devastating discovery that the data collected doesn’t match what the regulators need, forcing teams to restart expensive clinical trials.
This is where expert guidance becomes non-negotiable. Specialized consultants who understand the nuance of medical device development can help teams navigate the specific pathways for different classes of devices. For instance, understanding whether a device qualifies for the “Breakthrough Devices Program” can significantly speed up the review process. This designation is often available for devices that provide for more effective treatment of life-threatening or irreversibly debilitating human diseases. a category that many equity-focused innovations fall into.
The Data Gap and “Digital Twins”
Clinical trials are expensive and notoriously difficult to recruit for, often resulting in data sets that lack any kind of diversity. This creates a very vicious cycle where devices are approved based on skewed data, only to underperform in the broader population.
The Solution: But technology is providing a new answer in the form of “In Silico” trials, or Digital Twins. That means using advanced computer modeling to simulate how a device will interact with a vast range of virtual patient anatomies.
Instead of testing a heart valve on 50 people, developers can test it on 5,000 virtual hearts representing every age, size and pathology imaginable. While this doesn’t replace human trials, it allows engineers to “fail fast” and refine their designs in the virtual world before spending millions on physical prototypes. This technology is a game-changer for equity, as it allows for rigorous testing across diverse biological parameters that might be difficult to recruit for in a traditional study.
Designing for the Real World
Finally, a concept is only successful if it can actually be used in the intended environment. A high-tech diagnostic tool that requires consistent Wi-Fi and climate-controlled storage might work perfectly in a Boston teaching hospital, but it will fail in a rural clinic in the Delta or a mobile health unit.
The best solution is “Ruggedized Empathy.” Engineers must visit the environments where their devices will be used. They need to see the chaotic emergency rooms, the cramped mobile clinics and the homes of elderly patients. This on-the-ground reality check often leads to simpler, more robust and more intuitive designs that truly serve the mission of health equity.
Bringing a medical device to market is a monumental task. But by focusing on inclusive design, securing strategic funding and leveraging new technologies like digital simulation, innovators can ensure that their concepts survive the journey and, more importantly, that they work for everyone who needs them.
